Prior Authorization & Case Management
Haga clic aquí para ver esta información en español.
Beginning January 1, 2022, the Painters District Council No. 30 Health & Welfare Plan (Health Plan) will work with Valenz Care to implement and perform prior authorization and case management services. Plan participants were notified of these new Health Plan features at the start of 2022. The Health Plan has developed this page so participants can learn more about such questions as what is prior authorization and case management, how do these processes work, what is required of you and your providers, and what effect might these services have on your healthcare?
What are Prior Authorization and Case Management Services?
For participants in the PDC 30 Health Plan, a process commonly called prior authorization will be required for a variety of procedures, treatment plans, or other services recommended by your provider(s). Your providers may also use the terms “pre-authorization,” “pre-certification,” or “utilization review” to refer to prior authorization. Prior authorization is a requirement that your providers obtain approval from the Health Plan before performing a procedure, treatment plan, or other service. Without this prior approval, the Health Plan may not cover the claim submitted after this care was provided. Medical providers are very familiar with this process. Typically, they will know what they need to do in order to request prior authorization from a health plan or insurer, as this often involves treatment codes and other technical information. However, if there is any confusion, simply have your provider contact the PDC 30 Benefits Office.
The Health Plan requires prior authorization for procedures, treatment plans, or other services that relate to the treatment of a particular illness or injury, or the types of tests, imaging, or medical equipment associated with such conditions or diagnoses. This includes (but is not limited to) inpatient hospital admission, outpatient surgery, home health care, durable medical equipment, managed mental health care, and therapies in advance of admission or outpatient surgery. Valenz Care will assist you and your provider in determining what is subject to prior authorization, and what is not.
Case Management is intended to be a type of support service for participants and helps you navigate your healthcare during times of serious illness or injury, or earlier in your care when you appear to be contemplating a serious health matter. Case management can be implemented at various points in your care and may begin with prior authorization of procedures, treatment plans, or other services; it may also be initiated while you are receiving care for a particular condition that tends to be more complicated than other routine healthcare services. Valenz Care will match you with a dedicated Nurse Case Manager who coordinates care and guides you through procedures, treatment plans, or other services, so you can focus on returning to good health. There are several advantages of case management, such as:
- Minimizing out-of-pocket costs by ensuring you receive the right care at the right place at the right time
- Helping you coordinate and navigate your care across multiple care settings
- Monitoring and providing support during periods of rehabilitation and recovery
- Ensuring comprehensive care with one central point of contact
- Evaluating prescription drug regimens for safety, effectiveness, and lowest-cost options
If your medical condition warrants case management, a Nurse Case Manager will contact you promptly to begin care coordination. A participant must engage with case management services, which are provided at no additional cost to you.
What is Valenz Care? How to Contact?
 Valenz Care is a third-party prior authorization and case management service the Health Plan has selected to manage both prior authorization and case management processes. Therefore, if you receive letters from Valenz Care, you have either already discussed a serious medical procedure with your provider or may be in the process of seeking care that likely requires prior authorization and/or case management. You should carefully review these letters as if they are coming from the Health Plan, because the Health Plan will be working with Valenz Care to determine the medical necessity of procedures, treatment plans, or other services you are seeking. At times, letters from Valenz Care will require you and/or your doctor to provide additional medical information in order for your care to be considered for prior authorization and, subsequently, coverage by the Health Plan.
Valenz Care is a third-party prior authorization and case management service the Health Plan has selected to manage both prior authorization and case management processes. Therefore, if you receive letters from Valenz Care, you have either already discussed a serious medical procedure with your provider or may be in the process of seeking care that likely requires prior authorization and/or case management. You should carefully review these letters as if they are coming from the Health Plan, because the Health Plan will be working with Valenz Care to determine the medical necessity of procedures, treatment plans, or other services you are seeking. At times, letters from Valenz Care will require you and/or your doctor to provide additional medical information in order for your care to be considered for prior authorization and, subsequently, coverage by the Health Plan.
If you are seeking care that requires prior authorization, you will receive letters about that care directly from Valenz Care, and you and/or your provider should respond directly to Valenz Care if a request has been made for additional information. Questions about a specific prior authorization determination should also be made directly to Valenz Care and not the Health Plan.
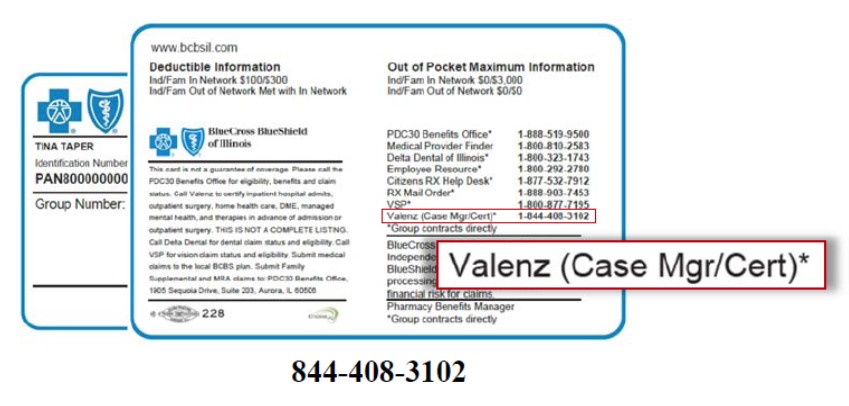
Contact Valenz Care at: 844-408-3102. This number is listed on the back side of your participant identification card (this is sometimes referred to as your Blue Cross/Blue Shield card).
Prior Auth / Case Mgmt: Questions & Answers
Will you still be able to choose your own doctors, specialists, and hospitals?
Why are these measures being adopted?
Can you appeal a determination not to authorize care?
Is prior authorization new?
For most eligible Health Plan participants at the start of 2022, the requirement that your provider submit care and treatment plans for prior authorization consideration is new. The Plan has always considered the medical necessity of your care in its determination of what is covered and what is not, and doctors and hospitals routinely contact the Benefits Office for authorization of care before they provide it. In order for the Health Plan to pay medical claims, care has always needed to be medically necessary; moreover, the amount the Plan pays for such care has always been limited to “usual, customary, and reasonable” (UCR) costs (and Health Plan participants have always been responsible for any charges that exceed UCR costs). The most significant change prior authorization will have is to position the review of medical necessity before such care is provided. This will help you avoid having to pay out-of-pocket for care that is not covered by the Plan.
Is case management new?
Case management has often been used by the Health Plan to assess the appropriateness of procedures, treatment plans, or other services provided to Plan participants, particularly when participants are addressing serious illness or injury, or receiving very complex and costly healthcare. Therefore, case management is not new to the Plan; however, at the start of 2022, case management and prior authorization together, facilitated by a single third-party provider (Valenz Care) is new. You should expect the processes will be highly efficient and timely, and will result in you receiving excellent care with fewer billing surprises. Valenz Care was selected to perform these services for the Health Plan because of their expertise and ability to provide high-quality service to you.
Will you still be able to choose your own doctors, specialists, and hospitals?
Yes; the use of prior authorization and case management will not alter the fundamental design of the PDC 30 Health Plan. The Health Plan offers you access to a contracted Preferred Provider Organization (PPO) network of providers and facilities (currently the Blue Cross Blue Shield of Illinois PPO network). You may also choose to receive care outside of this network, but you may be financially responsible for more of the costs of your care in such instances. When you use in-network providers, the Plan pays 90% of the costs for your care and you pay the remaining 10%, up to an annual out-of-pocket maximum of $3,000. You can go to a provider who is outside the BCBS of Illinois PPO network (an “out-of-network” provider); however, the Plan pays 85% of usual, customary, and reasonable costs for out-of-network care, and you are responsible for the remaining amount (and any amounts you pay out-of-pocket for out-of-network care are not applied to your annual out-of-pocket maximum). Prior authorization will be required for certain procedures, treatment plans, or other services for both in-network and out-of-network care. If you choose to consult with a specialist for a particular condition or concern, you will be able to do so without prior authorization; however, procedures, treatment plans, or other services recommended by that specialist may require prior authorization.
Case management is not new to the Health Plan; but, at the start of 2022, it will be utilized more uniformly in certain circumstances regardless of whether your care is provided by in-network or out-of-network providers. If your circumstances involve case management, you may learn more about your treatment options, which may help you avoid substantial out-of-pocket costs. For example, you may learn that aspects of your planned care involve a provider or facility that is out-of-network and you may be surprised to learn how much you will end up owing those providers after the Plan has paid its portion of a claim. As a result, you may decide to alter your plans and receive the same procedures, treatment plans, or other services through a provider or facility that is in-network.
Will prior authorization and/or case management cause delays in scheduling appointments and receiving medical care?
Even before using prior authorization, scheduling appointments for procedures, treatment plans, or other services recommended by providers already required several steps to verify eligibility, review coverages under participant plans, and schedule within available appointment times. Valenz Care has committed to reasonable timelines for review and will be working closely with the PDC 30 Health Plan in doing so. By calling Valenz Care, providers may learn immediately that no prior authorization is required for the particular care being recommended. Once initially notified by a provider in advance of the care being provided, if care requires prior authorization, Valenz Care will notify the provider of what is needed within one calendar day; following the receipt of the requested information in such a situation, timelines will depend on the urgency of the situation (delays caused by providers in responding to information requests may occur, but Valenz Care will do all that it can to encourage timely and complete responses). Complex procedures that are non-urgent may require requests for additional information, but Valenz Care is committed to response times that will be closely monitored by the Health Plan. If you find yourself in an emergency situation, prior authorization will not prevent you from receiving the emergency care providers believe is required at that time.
It is useful to keep in mind that prior authorization and case management are processes doctors and hospitals are VERY familiar with. They have office staff trained to process such authorizations. It is likely that you have experienced, or learned of, prior authorization and/or case management before, either through other health plans you have participated in, or plans that people you know participate in. Both are very common processes used by many health plans and are almost always a requirement of traditional health insurance plans. Valenz Care is widely used for these services by many health plans.
Is prior authorization and case management required? Must you and your providers work with Valenz Care?
When procedures, treatment plans, or other services require prior authorization, whether the PDC 30 Health Plan covers the cost of such care will be based significantly on Valenz Care’s determination of medical necessity. Participation in prior authorization and case management processes is a condition of consideration for coverage; refusal to participate in the review process when it is required will result in a denial of coverage of provider claims for the particular procedure, treatment, or other service that required prior authorization. As with all determinations of the Health Plan, you have the right to appeal coverage decisions to the Health Plan Board of Trustees.
During the provision of some types of medical care, the Health Plan’s coverage decisions will be significantly based on the guidance of Valenz Care’s case managers and related reviews of medical necessity conducted during your treatment. In addition to the many benefits to you of case management, you will find that prior authorization during on-going treatment for a serious illness or injury is more efficient when conducted in cooperation with case management than if sought outside of the case management process.
Why are these measures being adopted?
During 2020 and 2021, when the Board of Trustees of the PDC 30 Health & Welfare Plan determined the Health Plan would use prior authorization and expand its use of case management, the Health Plan was experiencing a record number of high-cost claims due to double-digit healthcare inflation and rapidly advancing and extremely expensive medical treatment options. At the same time, the Health Plan was reacting to the multifaceted impacts of the COVID-19 pandemic. These cost pressures were initially addressed, in 2020, when the PDC 30 Delegates determined they would temporarily reallocate a portion of the total hourly wage package that is typically contributed to the PDC 30 Pension Plan to the PDC 30 Health Plan. This measure, made possible because of the PDC 30 Pension Plan’s strong financial condition, was not intended to be a sustainable, long-term solution, but rather a temporary measure implemented while the Health Plan made some targeted structural changes. Processes such as prior authorization and case management seek to protect the most valuable benefits offered by the Plan to you, while making certain you can continue to receive increases in hourly wages and sustain other valuable benefits and member services (PDC 30’s Pension Plan, the MRA, the RSP, funding of its vital apprenticeship and training program [NCIFTI], and the advocacy and field presence of the District Council). In the interest of continuing to provide you and your family the highest quality medical coverage available, the logical response to these escalating costs is for the Plan to more closely monitor whether provider recommendations are medically necessary, what medical facilities are charging, and whether the costs of those services are within usual, customary, and reasonable ranges.
You also benefit from such monitoring by avoiding unnecessary medical procedures and treatment plans, by finding your way to the most effective providers for specialized care, by getting back to work and life more quickly, and by avoiding excessive out-of-pocket costs. Prior authorization and case management help you and your dependents make smart choices and avoid charges for care that the PDC 30 Health Plan does not cover. The Health Plan is a significant resource that, coupled with the PDC 30 Member Reimbursement Account (MRA), makes it possible for eligible PDC 30 members to cover their medical, prescription drug, dental, and vision expenses – reducing out-of-pocket costs as much as possible. Prior authorization and case management will provide you guidance during your care so you receive appropriate procedures, treatment plans, or other services within the same structure that has served PDC 30 members well for decades. Prior authorization and case management can also educate you on the conclusions being drawn by your providers, improving your understanding and ability to engage in thoughtful decision making concerning who provides you care, where the care is provided, when the care is provided, and how your recovery will work.
Can you appeal a determination not to authorize care?
Yes. If the prior authorization process results in a determination that certain procedures, treatment plans, or other services cannot be approved, these decisions can be appealed. There may also be situations when a provider submits incomplete information. Valenz Care will diligently pursue the information needed to review recommended care and facilitate any appeals; moreover, the PDC 30 Health Plan’s well-trained benefits specialists are available to answer your questions and concerns if the prior authorization and/or case management processes become confusing to you and/or your providers. As with all determinations of the Health Plan, if the prior authorization process determines recommended care to not be medically necessary, you have the right to appeal coverage decisions to the Health Plan Board of Trustees.